2 June 2020
Light on COVID-19
COVID-19 is a disease caused by the coronavirus SARS-CoV-2. It was first observed in humans in Wuhan, China, in December 2019 (hence the name). Remarkably, in November and December 2019, before the outbreak, a chiropractor in Orange County, California, posted on Facebook and in a private blog the claim that “heliotherapy” could be effective against a number of conditions, including infectious diseases. Heliotherapy is the attempted use of sun and daylight to cure infectious diseases of bacterial or lately also of viral origin. The question of course is whether irradiation by UV or other wavelengths of light is likely to prevent the spread of a newly discovered type of virus infection like COVID-19, or whether it makes a significant contribution rather later in the course, at the stages of healing and cure, once the infection is established, or makes no contribution at all. The answers depend on factors such as the location of the infectious agent in the body and the length of the incubation time during which the presence and spreading of the infectious agent may remain undetected and unguarded against. Pharmacological agents can play a role as well, also as an indirect agent of the sunlight, such as the case may be for vitamin D.
Early practitioners of heliotherapy, notably in the battle against epidemics, include the Danish-Faroese-Icelandic physician Niels Ryberg Finsen (1860-1904) (from a time when the kingdom encompassed all three locations) from Copenhagen, and the Swiss surgeon Auguste Rollier (1874-1954) from canton Vaud. Niels Finsen received the Nobel Prize in 1903 for his work on the focused light therapy of tuberculosis of the skin, the so-called lupus vulgaris. Auguste Rollier opened and operated a number of clinics in the Swiss alpine resort of Leysin, dedicated to the treatment of different forms of tuberculosis, particularly of bones, with ambient light from the sun shining on the southern slopes of the mountains near Montreux, evidently to considerable acclaim.
Tuberculosis is a bacterial infection of course but detailed knowledge of the differences between bacterial and viral agents did not arrive until late in the second half of the nineteenth century, about the time of the 8th International Medical Congress in Copenhagen in 1884, presided over by the Danish physician and physiologist Peter Ludvig Panum (1820-1885), and attended by such luminaries of infection and immunity fame as Louis Pasteur of France and Rudolph Virchow of Prussia.
Panum was an early observer of epidemics, first in the Faroe Islands in 1846 where he studied and effectively limited the spread of the virus of measles, and in 1850 in two provincial locations in continental Denmark where he was less successful at convincing the authorities that the bacterial epidemic of cholera that erupted there could be limited by quarantine. In the Faroe Islands, Panum determined the period of incubation of measles of two weeks and the salutary effects of quarantine, but in the case of the eruptions of cholera, he had difficulties proving the effect of isolation of the victims of cholera because of the widespread contamination of drinking water with fecal matter from patients, related to the dynamics of the local water supply (1).
It became clear that the use of isolation of inhabitants in cities with common exposures to environmental sources of infection would be a lot less effective than quarantines of individuals exposed to infection by direct association with other people. The point about the source of water was not widely appreciated, although it had just been reported by John Snow in a preliminary note in 1849, but more substantially not till 1853. Against Panum’s advice, the authorities lifted all quarantine measures for cholera in Denmark in 1852, and the result was not late in arriving. In 1853, cholera hit Copenhagen and surroundings, with at least 7000 cases and death rates of 70% at the focal point of a poorer part of Copenhagen. The culprits were soon shown to be the antiquated sources of drinking water and the ancient and dilapidated system of sewers in the city.
Of course, measles (morbilli, rubeola) is caused by the 100-150 nanometer wide paramyxovirus that is parasitic to humans but artificially infectious also to monkeys. COVID-19, on the other hand, is a very different affliction, caused by the 50-200 nanometer wide coronavirus SARS-CoV-2, one of many kinds of coronavirus. The incubation period is variable, about 2-14 days. This means that discussions of the proper procedures applicable to COVID-19 are not unlike the disagreements over the handling of epidemics in the second half of the nineteenth century.
The effects of focused light sources such as UV-light or exposure to sunlight or the elevated synthesis of vitamin D in the presence of sunlight are subjects of intense debate at the moment and the answers are at best uncertain. Papers on the topics are published at an increasing rate and include considerations of the effects of living in a sunny climate, effects of having your home architectonically designed to maximize the possible effects of daylight, and exploitations of the possible effects of increased vitamin D synthesis or supplementation.
In the example of France reported by Salje et al. (2), 3.6% of all infected individuals were hospitalized, and 0.7% of the infected individuals died, but with a wide range of mortality, ranging from 0.001% in those less than 20 years of age to as many as 10% of individuals aged more than 80. In France as elsewhere, significantly more men than women are hospitalized, enter intensive care, and die. The lockdown has been very effective and reduced the number of person-to-person infections from 3 physical associates to fewer than one on average. The question is what happens when lockdown and other interventions are lifted? Will the person-to-person infection rates simply rise again?
Both outdoor and indoor environments are linked to the seasonal distributions of respiratory infection by virus. The result is annual epidemics of common cold and influenza that erupt among humans in the winters of temperate climates, and the epidemics of SARS-CoV and SARS-CoV-2 are no exceptions, as noted by Moriyama et al. (3). The behavior of humans in relation to temperature and humidity of the surroundings is likely to affect the stability and transmission of respiratory virus, as well as the host’s immune response to infection of the respiratory tract.
Merow and Urban (4) claim that they are able to explain one-third of the variability of early countrywide growth rates of COVID-19, with one half of those cases depending on general weather conditions and environment, and the other half depending on factors specific to each country. They reported that ultraviolet light is the most important single factor associated with lower COVID-19 growth. This is taken to mean that the number of COVID-19 cases will decline in the summer and grow again by fall and winter, and that the heliotherapy of Auguste Rollier confirms the alleged impact of light from the sun. We know that approximately 5% of sunlight is ultraviolet radiation that reaches the surface of the globe, with the rest distributed more or less evenly between infrared and visible light. The effect of this radiation on the relation between duration of sunlight exposure and number of COVID-19 cases was exemplified in a study of incidence and death or recovery of cases in Jakarta, Indonesia. Here, Asyary and Veruswati (5) claim that the recovery of patients correlates significantly with the exposure to sunlight.
In the absence of much natural sunlight in places far from the Equator, as in the cases of temperate climates, it has been claimed that artificial so-called phototherapy can substitute for natural heliotherapy and thus reduce the impact of the coronavirus disease. There are a number of ways in which it may be possible to enlist modern light technology in the battles against COVID-19 and other infections, much like the violet-to-blue, 400–470 nm light that Niels Finsen chose for the treatment of tuberculosis. It is known that blue light inactivates several kinds of virus, including the coronavirus of influenza. In animals, red and near infrared light frequencies are also known to reduce respiratory disorders that are similar to complications from COVID-19 in people, and Enwemeka et al. (6) show that red light may reduce obstructive lung disease and bronchial asthma.
One of the important effects of light, and in particular sunlight, on humans is the production of vitamin D from a form of cholesterol in the skin. Vitamin D is converted to 1,25-dihydroxyvitamin D that is biologically active with numerous salutary effects (within limits) that suggest that light and sunlight may be important to human health through the production of vitamin D and its metabolites. There is now some evidence of a potential association between vitamin D and number of cases and death rates caused by COVID-19 in different countries. Thus, Ilie et al. (7) found inverse proportions between vitamin D in blood (average 56 mM) in each country and the number of COVID-19 cases per million in that country (average 300 cases/million). Vitamin D levels were reported to be so low in old people in Spain, Italy and Switzerland that they appear to join the groups most vulnerable to COVID-19.
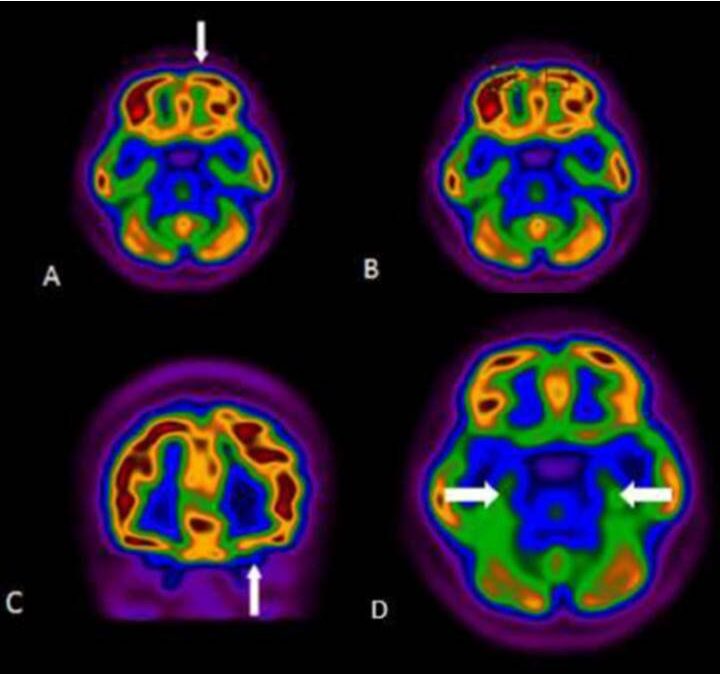
One of several possible reasons for the inverse association between vitamin D availability and the number of COVID-19 cases may be the known inhibition by vitamin D of an excessive immune response called the “cytokine storm”, with widespread consequences, including for brain function. It is an immune response so intense that it seems to destroy rather than protect the tissue. There is evidence of harmful effects of the cytokine storm in brain that mimic Parkinson’s disease, somewhat like the parkinsonism that many patients developed in the aftermath of the “Spanish” flu after the First World War (8, 9).
Another possible reason for the positive effects of vitamin D is the inhibition by 25-hydroxy-vitamin D of a transport mechanism that gives the SARS-CoV-2 virus access to the inside of tissues and cells in the human body. The transporter is an enzyme known as angiotensin-converting enzyme 2 (ACE2) that sits on cells as a kind of gateway to the interior. Without this transporter on the cell surface, the virus cannot gain access to the inside of cells. Current plans involve both the development of specific molecules that block the transporters, and the invention of drugs that remove the transporters from the cell surfaces and let them trap the virus outside the cells. In the latter case, it may actually be an advantage to have many more ACE2 molecules that in principle can float freely in the extracellular fluid and there trap the virus.
Significant health disparities exist between African and other Americans that render it of considerable interest to explore whether the difference may be related to the availability of vitamin D. In terms of COVID-19 hospitalization, the rate is now 2.4-fold higher for black Americans than for non-Hispanic white Americans. Grant and Peiris (10) reported an all-cause mortality rate for black Americans in 2006 that was 26% higher than for non-Hispanic white Americans, for reasons that previously were ascribed to socioeconomics, lifestyle, environment, and the access to health care. However, the authors claimed that these factors alone fail to account for the discrepancy and instead argued that it could be the higher serum 25-hydroxyvitamin D levels of white Americans that are responsible for their superior health. In the study, black Americans had an average serum 25-hydroxyvitamin D level of 40 mM, while white Americans had a value of 65 mM, a difference consistent with the relative mortality rates of the groups for breast cancer, colorectal cancer, and cardiovascular disease, as well as all-cause mortality, suggesting that low serum 25-hydroxyvitamin D availability remains an important health risk for African Americans, also with respect to the susceptibility to SARS-CoV-2 infection.
Finally, it is important to note the unsupported claim that treatment of COVID-19 with hydroxychloroquine, with or without the addition of azithromycin, can lower in-hospital mortality. The claim finds no support from scientific evidence. For example, for a group of 1438 patients hospitalized with COVID-19 in metropolitan New York, Rosenberg et al. (11) report that the in-hospital mortality was 20%, with no significant differences among patients receiving hydroxychloroquine, hydroxychloro-quine together with azithromycin, or azithromycin alone, or none of these drugs.
It is clear that issues abound, and that it is no scientifically fully confirmed hypothesis that UV-light, sunlight, or supplements related to vitamin D, make a difference. In contrast, it seems pretty clear that quarantine and isolation are the main reasons for the current decline in the total number of individuals with COVID-19 and the daily rates of new cases, hospitalizations, and deaths, suggesting that the numbers will start to rise again at the moment socialization is resumed on a global scale, unless herd immunity has intervened or a vaccine or other effective preventive drug such as an ACE2 inhibitor or ACE2 dislodging molecule becomes available.
References
- Gjedde A. [Peter Ludvig Panum’s Effort at Science]. Costers 1971, 256 pp. https://bibliotek.dk/linkme.php?rec.id=870970-basis%3A07565631
- Salje H, Tran Kiem C, Lefrancq N, Courtejoie N, Bosetti P, Paireau J, Andronico A, Hozé N, Richet J, Dubost CL, Le Strat Y, Lessler J, Levy-Bruhl D, Fontanet A, Opatowski L, Boelle PY, Cauchemez S. Estimating the burden of SARS-CoV-2 in France. Science. 2020 May 13. pii: eabc3517. doi: https://doi.org/10.1126/science.abc3517. [Epub ahead of print] PubMed PMID: 32404476
- Moriyama M, Hugentobler WJ, Iwasaki A. Seasonality of Respiratory Viral Infections Rev. Virol. 2020. 7:2.1–2.19 virology.annualreviews.org https://doi.org/10.1146/annurev-virology-012420-022445
- Merow C, Urban MC. Seasonality and uncertainty in COVID-19 growth rates. medRxiv preprint doi: https://doi.org/10.1101/2020.04.19.20071951, version posted April 22, 2020.
- Asyary A, Veruswati M. Sunlight exposure increased Covid-19 recovery rates: A study in the central pandemic area of Indonesia. Sci Total Environ. 2020 Apr 27; 729: 139016. doi: https://doi.org/10.1016/j.scitotenv.2020.139016. [Epub ahead of print] PubMed PMID: 32361458.
- Enwemeka CS, Bumah VV, Masson-Meyers DS. Light as a potential treatment for pandemic coronavirus infections: A perspective. Journal of Photochemistry & Photobiology, B: Biology JPB 111891 PII: S1011-1344(20)30341-9. doi: https://doi.org/10.1016/j.jphotobiol.2020.111891.
- Ilie PC, Stefanescu S, Smith L. The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality. Aging Clin Exp Res. 2020 May 6. doi: https://doi.org/10.1007/s40520-020-01570-8. [Epub ahead of print] PubMed PMID: 32377965; PubMed Central PMCID: PMC7202265.
- Victorino DB, Guimaraes-Marques M, Nejm M, Scorza FA, Scorza CA. COVID-19 and Parkinson’s disease: Are we dealing with short-term impacts or something worse? Journal of Parkinson’s Disease doi: https://doi.org/10.3233/JPD-202073.
- Coolen T, Lolli V, Sadeghi N, Rovaï A, Trotta N, Taccone FS, Creteur J, Henrard S, Goffard JC, DeWitte O, Naeije G, Goldman S, DeTiège X. Early postmortem brain MRI findings in COVID-19 non-survivors. medRxiv preprint: https://www.medrxiv.org/content/10.1101/2020.05.04.20090316v1.
- Grant WB, Peiris AN. Possible role of serum 25-hydroxyvitamin D in black-white health disparities in the United States. J Am Med Dir Assoc. 2010 Nov;11(9):617-28. doi: https://doi.org/10.1016/j.jamda.2010.03.013. Review. PubMed PMID: 21029996.
- Rosenberg ES, Dufort EM, Udo T, Wilberschied LA, Kumar J, Tesoriero J, Weinberg P, Kirkwood J, Muse A, DeHovitz J, Blog DS, Hutton B, Holtgrave DR, Zucker HA. Association of treatment with hydroxychloroquine or azithromycin with in-hospital mortality in patients with COVID-19 in New York State. JAMA. 2020 May 11. doi: https://doi.org/10.1001/jama.2020.8630. [Epub ahead of print] PubMed PMID: 32392282

Very interesting article, much of this might be true.